The goal of the medical biller is to ensure that the provider is properly reimbursed for their services. In the pursuit of this goal, errors, both human and electronic, are unfortunately unavoidable. Since the process of medical billing involves two incredibly important elements (namely, health and money), it’s important to reduce as many of these errors as possible. In this brief course, we’ll introduce you to some common errors in the medical billing practice.
Before we jump into that discussion, however, let’s review the difference between a rejected and denied claim.
Denied and Rejected Claims
As you’ll recall from previous Courses, a rejected claim is not the same as a denied one. A rejected claim is one that contains one or many errors found before the claim is processed. These errors prevent the insurance company from paying the bill as it is composed, and the rejected claim is returned to the biller in order to be corrected. A rejected claim may be the result of a clerical error, or it may come down to mismatched procedure and ICD codes. A rejected claim will be returned to the biller with an explanation of the error. These claims are then corrected and resubmitted.
Clearinghouses employ a process called “scrubbing” in order to avoid rejected claims. The end goal, for billers and clearinghouses, is a “clean” claim.
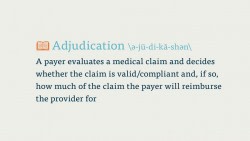
Denied claims, on the other hand, are claims that the payer has processed and deemed unpayable. These claims may violate the terms of the payer-patient contract, or they may just contain some sort of vital error that was only caught after processing. Payers will include an explanation for why a claim is denied when they send the denied claim back to the biller. Many times, these claims can be appealed and sent back to the payer for processing, but this process can be time-consuming and, therefore, costly. For that reason, it’s important to try and get as many claims “clean” on the first go, and not waste any time billing for procedures that are incompatible with a patient’s coverage.
Simple Errors
Now that we’ve reviewed denied and rejected claims, let’s look at some of the basic errors that can get a claim returned to the biller.
Incorrect patient information
Sex, name, DOB, insurance ID number, etc.
Incorrect provider information
Address, name, contact information, etc.
Incorrect Insurance provider information
Wrong policy number, address, etc
Incorrect codes
Entering confusing ICD, CPT, or HPCS codes; entering confusing Place of Service codes; attaching conflicting or confusing modifiers to HCPCS or CPT codes; entering too few or too many digits to an ICD, CPT, or HCPCS codes
Mismatched medical codes
Entering confusing ICD codes with CPT codes, or vice versa, etc
Leaving out codes altogether for procedures or diagnoses
Duplicate Billing
This occurs when someone at the provider’s office submits a claim for a procedure without checking whether that service has been paid for/reported. Duplicate billing can create a huge headache for billers and payers alike, because it may appear that a patient received two identical x-rays on one day, which would effectively double the amount sent to the payer.
Like medical coding, we’re always striving for the highest level of accuracy in our codes, and we’re also required to provide as complete a picture as possible of the medical procedure(s). If you can cut down on these simple errors in your medical billing, you’ll have a much higher number of clean claims.
More Billing Errors
The above are some of the most frequent errors a medical biller comes across. These errors directly affect the status of a claim, which makes them very important to watch out for.
But there are other errors to watch out for as you go through your day as a medical biller. Some of these are, regrettably, out of the biller’s hands, but they’re important to watch out for nonetheless.
Undercoding
Undercoding occurs when a provider intentionally leaves out a procedure code from a superbill, or codes for a less serious or extensive procedure than the patient received. Undercoding may be done to avoid audits for certain procedures, or to try and save money for the patient. This process is illegal, and counts as a type of fraud.
Upcoding
Like undercoding, this is a fraudulent process wherein the provider intentionally misrepresents the work they performed on a patient. In upcoding, a practice enters codes for services a patient did not receive, or codes for more intensive procedures then the provider actually performed. Upcoding is typically done in an attempt to receive more money from a payer. This, like undercoding, is a fraudulent practice, and should be noted and reported immediately.
Poor documentation
While not a fraudulent practice like upcoding or undercoding, poor documentation can also negatively affect the claims process. If a provider has provided incorrect, illegible, or incomplete documentation of a procedure or patient visit, it’s difficult to make an accurate or complete claim. In cases of sloppy documentation, the biller should contact the provider and ask for more information.
No EOB on denied claim
In certain cases, the payer may fail to attach the Explanation of Benefits (EOB) to a denied claim. In cases like this, it’s difficult to note the error on a denied claim, which slows down the (already slow) appeals process.
Fixing Errors Before They Happen
It’s always important to be proactive when you’re medical billing. Here are a few of things you can do to catch medical billing errors before they happen.
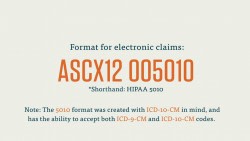
Stay Current
Billers need to stay up-to-date on billing and coding trends. Coding especially will change as new codes are introduced and older ones phased out. It’s important to check on new protocols in medical coding regularly. Study new codes and be aware of how they affect billing.
Be Diligent
You should always double check your work when you’re creating a claim. Simple clerical errors like missing digits or misspelled names can be the difference between an approved and a rejected claim, so go over each claim you create before you send it off.
Communicate
Part of reducing medical billing errors comes down to coordinating effectively within the provider’s office. Make sure you communicate regularly and effectively with other personnel in the provider’s office, including the physician, and don’t be afraid to ask questions about possible errors on the claim.
Follow Through
After you send a claim in to a payer, you can follow up with a representative working on that claim. They may be able to alert you to any errors they’ve already caught, in which case you can begin work on making a new, error-free claim. (Wait until they send it back to you, of course!)